What Is Bursitis On The Feet?
Heel bursitis is specifically the inflammation of the retrocalcaneal bursa, located at the back of the heel, under the Achilles tendon. There are a handful of factors that put you at risk for developing heel bursitis. Long distance runners are prone to heel bursitis, due to repeated stress and pounding upon the heel joint. Engaging in activities such as running, bicycling, walking, jumping, and stair climbing for extended periods of time can overwork the heel joints and start to irritate the bursae. Suddenly changing to a high-intensity workout regime puts a lot of stress on the heel, making it vulnerable to injury. Hard blows/bumps to the heel can immediately damage the bursae, leading to swelling and inflammation. Training at high intensities without stretching and warming up can also contribute to the development of heel bursitis. Even improper footwear can be a big factor. Some other conditions can put you at risk as well, such as: tarsal tunnel syndrome, rheumatoid arthritis, plantar fasciitis, muscle weakness, joint stiffness, and heel spurs. It is very important to get a professional diagnosis if you are having heel pain because heel bursitis is often confused for Achilles tendonitis, and the proper treatments are very different. The pain could also be plantar fasciitis or general heel pain syndrome.
Causes
Overtraining in a runner (eg, excessive increases in miles or intensity). Tight or poorly fitting shoes that, because of a restrictive heel counter, exert excessive pressure on the posterior heel and ankle
Haglund deformity, causing impingement between the increased posterior superior calcaneal prominence and the Achilles tendon during dorsiflexion. More recent research suggests that a misaligned subtalar joint axis (measured in terms of joint inclination and deviation) in relation to the Achilles tendon can result in an asymmetrical force load on the tendon, disrupting normal biomechanics. This altered joint axis is associated with an increased risk for Achilles pathologies, including bursitis.
Symptoms
A dull ache under the heel when not weight bearing. Sometimes severe pain when walking. Pain can increase after resting (sleeping or sitting) then standing and placing pressure on the area again. Throbbing under the heel. Swelling may be identified as a discernible lump under the heel. This is the swollen calcaneal bursa itself. Tingling under the heel as swelling affect the plantar nerves. Pains shooting into the foot or up the leg.
Diagnosis
A physical examination will be performed to determine if you have any signs of Achilles Bursitis or other ankle injury. He/she will look and feel the soft tissue and bones in your ankles to note any differences between the two of them. This will identify any abnormalities, such as swelling, bone deformities, atrophied muscles, redness and/or warmth on the skin. In many cases, the first sign that you have Achilles bursitis is swelling in the back of the foot and ankle pain.
Non Surgical Treatment
With anterior and posterior Achilles tendon bursitis, applying warm or cool compresses to the area and using nonsteroidal anti-inflammatory drugs (NSAIDs) can temporarily relieve the pain and inflammation, as can injections of a corticosteroid/anesthetic mixture into the inflamed bursa. The doctor is careful not to inject the mixture into the tendon. After this treatment, the person should rest. When these treatments are not effective, part of the heel bone may need to be surgically removed.
Surgical Treatment
Surgery is rarely need to treat most of these conditions. A patient with a soft tissue rheumatic syndrome may need surgery, however, if problems persist and other treatment methods do not help symptoms.
Prevention
Maintain proper form when exercising, good flexibility, and strength around the ankle to help prevent this condition from arising. Proper stretching of the achilles tendon helps prevent injury.
Hammer Toe Treatment In The Home
 Overview
Overview
A hammertoes is a toe that is contracted at the PIP joint (middle joint in the toe), potentially leading to severe pressure and pain. Ligaments and tendons that have tightened cause the toe's joints to curl downwards. Hammer toes may occur in any toe except the big toe. There is often discomfort at the top part of the toe due to rubbing against the shoe.
Causes
A hammertoe is formed due an abnormal balance of the muscles in the toes. This abnormal balance causes increased pressures on the tendons and joints of the toe, leading to its contracture. Heredity and trauma can also lead to the formation of a hammertoe. Arthritis is another factor, because the balance around the toe in people with arthritis is so disrupted that a hammertoe may develop. Wearing shoes that are too tight and cause the toes to squeeze can also be a cause for a hammertoe to form.
 Symptoms
Symptoms
Signs and symptoms of hammertoe and mallet toe may include a hammer-like or claw-like appearance of a toe. In mallet toe, a deformity at the end of the toe, giving the toe a mallet-like appearance. Pain and difficulty moving the toe. Corns and calluses resulting from the toe rubbing against the inside of your footwear. Both hammertoe and mallet toe can cause pain with walking and other foot movements.
Diagnosis
Hammer toes may be easily detected through observation. The malformation of the person's toes begin as mild distortions, yet may worsen over time - especially if the factors causing the hammer toes are not eased or removed. If the condition is paid attention to early enough, the person's toes may not be permanently damaged and may be treated without having to receive surgical intervention. If the person's toes remain untreated for too long, however the muscles within the toes might stiffen even more and will require invasive procedures to correct the deformity.
Non Surgical Treatment
In the earlier stages of hammer toe, when the toes can still be manually straightened, then conservative treatment is appropriate. This means wearing shoes which are a half size bigger than normal and which are not narrow around the toes. Exercises to stretch the toes out and strengthen the muscles under the foot which balances the tightness of the top tendons are important. Padding or corn plasters can be used to ease the discomfort of any associated corns and calluses.
Surgical Treatment
Curative Hammer toe treatment of hammertoes varies depending upon the severity of the deformity. When the hammertoe is flexible, a simple tendon release in the toe works well. The recovery is rapid often requiring nothing more that a single stitch and a Band-Aid. Of course if several toes are done at the same time, the recovery make take a bit longer.
 Prevention
Prevention
Few people realize that their feet grow over the years: actually, the heel stays the same, but the front of the foot becomes wider and longer. The result, most women wear shoes that fit at the heel but are much too narrow in the front. Buy shoes that fit the longer foot. For two out of three people, one foot is significantly bigger than the other. Have both feet measured whenever you buy shoes. Have your feet measured while you're standing, and buy shoes that fit the larger foot. Shop at the end of the day, when foot swelling is greatest. No shoe should feel tight. Don't go by numbers. You may think of yourself as a size 8B, but size varies from shoe to shoe. There is no standardization, so pick the shoes that fit best. Limit high-heel use. These shoes increase pressure on the front of the foot by at least 50 percent, so wear them only for special occasions. Flat shoes are more comfortable than high heels, but they, too, can be hard on your feet, especially if they are thin-soled. Change your shoes. If your shoes are too short or too narrow, get another pair. This is especially important for children going through periods of rapid growth. The toe area should be high enough so that it doesn't rub against the top of your toes-especially if hammer toes have started to develop.
Bunions Causes Warning Signs And Treatments
Overview
 Bunion is the common term for a medical condition known as Hallux Valgus. Hallux Valgus is the tilting of the toe away from the mid-line of the body. It is usually characterized by a lump or bump that is red, swollen and/or painful on the inside of the foot in and around the big toe joint.
Bunion is the common term for a medical condition known as Hallux Valgus. Hallux Valgus is the tilting of the toe away from the mid-line of the body. It is usually characterized by a lump or bump that is red, swollen and/or painful on the inside of the foot in and around the big toe joint.
Causes
Bunions are most often caused by faulty foot mechanics. It is not the bunion itself that is inherited, but certain foot types that make a person prone to developing a bunion. Although wearing shoes that crowd the toes won't actually cause bunions in the first place, it sometimes makes the deformity progressively worse. That means you may experience symptoms sooner.
Symptoms
Bunions are an often painful condition that may become even more painful as extra bone and a fluid-filled sac grow at the base of your big toe. Some of the most frequently experienced signs and symptoms associated with bunions, besides pain, include redness in your affected area. Blistering over your bunion. Callus formation around your bunion. Bursitis. Nerve damage (numbness and/or sharp pains) in your involved area. Bunions may also cause pain within and below your first metatarsophalangeal, or MTP, joint. Your bunion may become further dislocated and unstable as it progresses and may overload your adjacent joints.
Diagnosis
A doctor can very often diagnose a bunion by looking at it. A foot x-ray can show an abnormal angle between the big toe and the foot. In some cases, arthritis may also be seen.
Non Surgical Treatment
You can buy orthotics over the counter from pharmacies, or they can be custom-made by a podiatrist to fit your feet. Whether you need to buy an over-the-counter orthotic or have one specially made will depend on your individual circumstances and the severity of your bunion. You can also use special bunion splints, worn over the top of your foot and your big toe to help straighten its alignment. Splints are available for both daytime and night-time use. However, there's little evidence that splints are effective. Toe spacers are also available, which can help reduce the pain caused by bunions. However, toe spacers or orthotics may be of limited use because they often compete with the bunion for the already limited space in the shoe. If your toe joint is painful and swollen, applying an ice pack to the affected area several times a day can help to relieve the pain and inflammation. Never apply ice directly to your skin. Wrap it in a cloth or tea towel. A bag of frozen vegetables makes a good ice pack. It's recommended that you wear flat or low-heeled, wide-fitting shoes if you have a bunion. Shoes made from soft leather are ideal because they'll relieve any pressure on the bunion. Avoid narrow or slip-on shoes. High heels can also make your bunion worse by putting excessive pressure on your toes. 
Surgical Treatment
There is no "standard" bunion, but rather a complex range of joint, bone, muscle, tendon and ligament abnormalities that can cause variation in each bunion's make-up. As a result, there are a broad variety of surgical techniques for dealing with bunions. Most surgical procedures start with a simple bunionectomy, which involves excision of swollen tissues and removal of the enlarged boney structure. While this may remove the troublesome tissues, however, it may not correct other issues associated with the bunion. The surgeon may also need to tighten or loosen the muscles, tendons and ligaments around the MTP joint. Realign the bone by cutting it and shifting its position (a technique called osteotomy), realigning muscles, tendons and ligaments accordingly. Use screws, wires or plates to hold the joint surfaces together until they heal. Reconstruct a badly damaged joint or replace it with an artificial implant.
Does Overpronation Of The Feet Need An Operation
While a slight amount of pronation is the proper means to absorb shock naturally, too much pronation (over-pronation) can potentially contribute to many maladies, which can sideline a runner. A foot that pronates excessively is one that continues to roll inward past a neutral position after the shock of impact has been absorbed. Uncorrected and repeated, this motion may lead to repetitive stress related injuries of the feet and legs. More times than not, the runner who over-pronates needs a shoe that reduces excess pronation and guides the foot along a neutral path.
Causes
There is a relationship between biomechanics and injury that is specific to each body part. Overall though, poor mechanics will either increase the landing forces acting on the body or increase the work to be done by the muscles. Both increase the stress, which, depending on the individual and the amount of running can become excessive and cause injury.
Symptoms
When standing, your heels lean inward. When standing, one or both of your knee caps turn inward. Conditions such as a flat feet or bunions may occur. You develop knee pain when you are active or involved in athletics. The knee pain slowly goes away when you rest. You abnormally wear out the soles and heels of your shoes very quickly.
Diagnosis
You can test for pronation by looking at the leg and foot from the back. Normally you can see the Achilles Tendon run straight down the leg into the heel. If the foot is pronated, the tendon will run straight down the leg, but when it lies on the heel it will twist outward. This makes the inner ankle bone much more prominent than the outer ankle bone.
Non Surgical Treatment
Wear shoes with straight or semicurved lasts. Motion-control or stability shoes with firm, multidensity midsoles and external control features that limit pronation are best. Over-the-counter orthotics or arch supports can help, too. You know you are making improvements when the wear pattern on your shoes becomes more normal. Overpronation causes extra stress and tightness to the muscles, so do a little extra stretching.
Surgical Treatment
The MBA implant is small titanium device that is inserted surgically into a small opening between the bones in the hind-mid foot: the talus (ankle bone) and the calcaneus (heel bone). The implant was developed to help restore the arch by acting as a mechanical block that prevents the foot from rolling-in (pronation). In the medical literature, the success rate for relief of pain is about 65-70%. Unfortunately, about 40% of people require surgical removal of the implant due to pain.
Severs Disease Physical Therapy
Sever?s disease is caused by the growth plate in the heel becoming inflamed, and it is the most common cause of heel pain in adolescents. This condition is especially prevalent in children who play sports. Treatment includes ice, rest, and pain relievers to manage pain and discomfort. Any underlying foot conditions may also need to be assessed and managed. Sever?s disease does not cause any permanent damage, and will resolve when the growth of the heel is complete. Sever?s disease (also called calcaneal apophysitis) is a condition that occurs in the growth plate of the heel bone (the calcaneus) in children and adolescents. When the muscles and tendons in the leg and heel exert too much pressure on this growth plate, swelling and pain can result.
Causes
The heel bone sometimes grows faster than the leg muscles (including the calf muscles) and tendons (including the Achilles tendon) during the early puberty growth spurt. The different growth rate in these structures can cause lower leg muscles and tendons to become overstretched and tight, which makes the heel less flexible and puts excessive pressure on the heel growth plate. The Achilles tendon, the strongest tendon in the body, attaches to the heel growth plate, and repetitive stress on this structure, especially if it?s already tight, can damage the growth plate, leading to tenderness, swelling, and pain. Activities that involve running or jumping, such as soccer, gymnastics, track, and basketball, can place significant stress on a tight Achilles tendon and contribute to the onset of Sever?s disease. Ill-fitting shoes can also contribute to this health problem by failing to provide the right kind of support or by rubbing against the back of heel. The following factors may increase the likelihood of Sever?s disease in kids or young teens. Wearing footwear that is too narrow in the toe box. Leg length inequality. Obesity or carrying excess bodyweight. Excessive foot and ankle pronation.
Symptoms
Symptoms include Heel Pain. Pain at the back of the heels when walking or running. Possibly a lump at the back of the heel, although this might be minimal. Pain and tenderness at the back of the heels, especially if you press on it, or give it a squeeze from the sides. Tight calf muscles resulting in reduced ankle range of motion.
Diagnosis
This condition is self limiting, it will go away when the two parts of bony growth join together, this is natural. Unfortunately, Sever's disease can be very painful and limit sport activity of the child while waiting for it to go away, so treatment is often advised to help relieve it. In a few cases of Sever's disease, the treatment is not successful and these children will be restricted in their activity levels until the two growth areas join, usually around the age of 16 years. There are no known long term complications associated with Sever's disease.
Non Surgical Treatment
Treatment for Sever?s disease is mainly supportive, to stop inflammation and reduce pain. The condition will resolve on its own when the growth in the growth plate is complete, but until then, measures can be taken to resolve pain and discomfort. Applying ice to the painful or swollen areas on the foot may provide some short-term relief from pain and prevent further inflammation. Ice can be applied for about 20 minutes two or three times a day. Footwear that is too big, too small, or does not provide proper support can exacerbate the symptoms of Sever?s disease. Supportive footwear is important to prevent discomfort, especially in children who participate in sports and activities that take place on a hard surface (such as pavement or a basketball court). Shoes should also have adequate padding and not rub against the heel. In some cases, shoes that do not have heels (such as sandals) may be more comfortable to wear while the heel is healing, but care should be taken that the shoe provides proper support to the rest of the foot. Children with Sever?s disease should avoid going barefoot.Children with flat feet, high arches, or over-pronation may need treatment to resolve these underlying conditions. In many cases, an orthotic worn inside the shoe can help put the foot into a better alignment and provide relief to the foot or the arch. Children who are overweight or obese may be counseled to lose weight. Being overweight can contribute to the development of several conditions, including Sever?s disease. Resting the foot and discontinuing sports and other activities until the pain and stiffness is resolved may be recommended. In extreme cases, a walking boot or a cast might be used to completely immobilize the foot. A physical therapist may recommend stretching exercises for the muscles in the calf and the Achilles tendon. A stretching routine is usually done several times a day. Stretching these muscles can help improve strength and decrease the stress on the heel plate. Some physicians may recommend over-the-counter pain relievers such as ibuprofen or acetaminophen. Care must be taken when administering these medications to children, especially with acetaminophen, as overdoses are possible when using more than one medication containing acetaminophen. Aspirin should never be given to children. The utility of pain relievers in children must be weighed against their possible side effects. For small variations-less than an inch or so-shoe lifts can help equalize the length of the legs. In cases with more variation between legs, surgical solutions may be considered. Research indicates that targeted manual therapy techniques performed by a licensed physical therapist can help to reduce pain from Sever?s Disease and to improve muscle function. When the larger calf muscles and the smaller ankle and foot muscles become tight, this tightness can affect the mechanics of the ankle joint. Manual therapy includes both joint and muscle release techniques to restore optimal function to the calf, ankle, and foot muscles, and results can generally be achieved within a few months.
Exercise
The following exercises are commonly prescribed to patients with Severs disease. You should discuss the suitability of these exercises with your physiotherapist prior to beginning them. Generally, they should be performed 1 - 3 times daily and only provided they do not cause or increase symptoms. Your physiotherapist can advise when it is appropriate to begin the initial exercises and eventually progress to the intermediate, advanced and other exercises. As a general rule, addition of exercises or progression to more advanced exercises should take place provided there is no increase in symptoms. Calf Stretch with Towel. Begin this stretch in long sitting with your leg to be stretched in front of you. Your knee and back should be straight and a towel or rigid band placed around your foot as demonstrated. Using your foot, ankle and the towel, bring your toes towards your head as far as you can go without pain and provided you feel no more than a mild to moderate stretch in the back of your calf, Achilles tendon or leg. Hold for 5 seconds and repeat 10 times at a mild to moderate stretch provided the exercise is pain free. Calf Stretch with Towel. Begin this exercise with a resistance band around your foot and your foot and ankle held up towards your head. Slowly move your foot and ankle down against the resistance band as far as possible and comfortable without pain, tightening your calf muscle. Very slowly return back to the starting position. Repeat 10 - 20 times provided the exercise is pain free. Once you can perform 20 repetitions consistently without pain, the exercise can be progressed by gradually increasing the resistance of the band provided there is no increase in symptoms. Bridging. Begin this exercise lying on your back in the position demonstrated. Slowly lift your bottom pushing through your feet, until your knees, hips and shoulders are in a straight line. Tighten your bottom muscles (gluteals) as you do this. Hold for 2 seconds then slowly lower your bottom back down. Repeat 10 times provided the exercise is pain free.
Chronic Achilles Tendon Rupture Treatment
Overview
 Pain of the Achilles tendon commonly affects both competitive and recreational athletes, and the sedentary. The largest tendon in the body, the Achilles tendon, endures strain and risks rupture from running, jumping, and sudden acceleration or deceleration. Overuse, vascular diseases, neuropathy, and rheumatologic diseases may cause tendon degeneration. The hallmarks of Achilles tendon problems seem to be damaged, weak, inelastic tissue.
Pain of the Achilles tendon commonly affects both competitive and recreational athletes, and the sedentary. The largest tendon in the body, the Achilles tendon, endures strain and risks rupture from running, jumping, and sudden acceleration or deceleration. Overuse, vascular diseases, neuropathy, and rheumatologic diseases may cause tendon degeneration. The hallmarks of Achilles tendon problems seem to be damaged, weak, inelastic tissue.
Causes
As with any muscle or tendon in the body, the Achilles tendon can be torn if there is a high force or stress on it. This can happen with activities which involve a forceful push off with the foot, for example, in football, running, basketball, diving, and tennis. The push off movement uses a strong contraction of the calf muscles which can stress the Achilles tendon too much. The Achilles tendon can also be damaged by injuries such as falls, if the foot is suddenly forced into an upward-pointing position, this movement stretches the tendon. Another possible injury is a deep cut at the back of the ankle, which might go into the tendon. Sometimes the Achilles tendon is weak, making it more prone to rupture. Factors that weaken the Achilles tendon are corticosteroid medication (such as prednisolone), mainly if it is used as long-term treatment rather than a short course. Corticosteroid injection near the Achilles tendon. Certain rare medical conditions, such as Cushing?s syndrome, where the body makes too much of its own corticosteroid hormones. Increasing age. Tendonitis (inflammation) of the Achilles tendon. Other medical conditions which can make the tendon more prone to rupture, for example, rheumatoid arthritis, gout and systemic lupus erythematosus (SLE) - lupus. Certain antibiotic medicines may slightly increase the risk of having an Achilles tendon rupture. These are the quinolone antibiotics such as ciprofloxacin and ofloxacin. The risk of having an Achilles tendon rupture with these antibiotics is actually very low, and mainly applies if you are also taking corticosteroid medication or are over the age of about 60.
Symptoms
You may notice the symptoms come on suddenly during a sporting activity or injury. You might hear a snap or feel a sudden sharp pain when the tendon is torn. The sharp pain usually settles quickly, although there may be some aching at the back of the lower leg. After the injury, the usual symptoms are as follows. A flat-footed type of walk. You can walk and bear weight, but cannot push off the ground properly on the side where the tendon is ruptured. Inability to stand on tiptoe. If the tendon is completely torn, you may feel a gap just above the back of the heel. However, if there is bruising then the swelling may disguise the gap. If you suspect an Achilles tendon rupture, it is best to see a doctor urgently, because the tendon heals better if treated sooner rather than later.
Diagnosis
A doctor will look at the type of physical activity you have been doing. He or she will then look at your foot, ankle and leg. An MRI may also be used. This is to help determine the severity of the tear and the extent of separation of the fibers.
Non Surgical Treatment
Non-surgical management traditionally was selected for minor ruptures, less active patients, and those with medical conditions that prevent them from undergoing surgery. It traditionally consisted of restriction in a plaster cast for six to eight weeks with the foot pointed downwards (to oppose the ends of the ruptured tendon). But recent studies have produced superior results with much more rapid rehabilitation in fixed or hinged boots. 
Surgical Treatment
Most published reports on surgical treatment fall into 3 different surgical approach categories that include the following: direct open, minimally invasive, and percutaneous. In multiple studies surgical treatment has demonstrated a lower rate of re-rupture compared to nonoperative treatment, but surgical treatment is associated with a higher rate of wound healing problems, infection, postoperative pain, adhesions, and nerve damage. Most commonly the direct open approach involves a 10- to 18-cm posteromedial incision. The minimally invasive approach has a 3- to 10-cm incision, and the percutaneous approach involves repairing the tendon through multiple small incisions. As with nonsurgical treatment there exists wide variation in the reported literature regarding postoperative treatment protocols. Multiple comparative studies have been published comparing different surgical approaches, repair methods, or postoperative treatment protocols.
Prevention
Here are some suggestions to help to prevent this injury. Corticosteroid medication such as prednisolone, should be used carefully and the dose should be reduced if possible. But note that there are many conditions where corticosteroid medication is important or lifesaving. Quinolone antibiotics should be used carefully in people aged over 60 or who are taking steroids.
What Exactly Is Posterior Tibial Tendon Dysfunction ?
Overview
Another common term for this condition is Posterior Tibial Tendon Dysfunction (PTTD). There is a cause-effect relationship between pronation, flatfoot deformity and subsequent tenosynovitis of the posterior tibial tendon. Mechanical irritation of the tendon may lead to synovitis, partial tearing and eventually full rupture of the tendon. Other structures, including ligaments and the plantar fascia, have also been shown to contribute to the arch collapsing. As the deformity progresses, these structures have been shown to attenuate and rupture as well. In later stages, subluxation of various joints lead to a valgus rearfoot and transverse plane deformity of the forefoot. These deformities can become fixed and irreducible as significant osteoarthritis sets in. 
Causes
Flat feet causes greater pressure on the posterior tibial tendon than normal. As the person with flat feet ages, the muscles, tendons and ligaments weaken. Blood supplies diminish as arteries narrow. These conditions are magnified for obese patients because of their increased weight and atherosclerosis. Finally, the tendon gives out or tears. Most of the time, this is a slow process. Once the posterior tibial tendon and ligaments stretch, body weight causes the bones of the arch to move out of position. The foot rotates inward (pronation), the heel bone is tilted to the inside, and the arch appears collapsed. In some cases, the deformity progresses until the foot dislocates outward from the ankle joint.
Symptoms
Symptoms are minor and may go unnoticed, Pain dominates, rather than deformity. Minor swelling may be visible along the course of the tendon. Pain and swelling along the course of the tendon. Visible decrease in arch height. Aduction of the forefoot on rearfoot. Subluxed tali and navicular joints. Deformation at this point is still flexible. Considerable deformity and weakness. Significant pain. Arthritic changes in the tarsal joints. Deformation at this point is rigid.
Diagnosis
Observation by a skilled foot clinician and a hands-on evaluation of the foot and ankle is the most accurate diagnostic technique. Your Dallas foot doctor may have you do a walking examination (the most reliable way to check for the deformity). During walking, the affected foot appears more pronated and deformed. Your podiatrist may do muscle testing to look for strength deficiencies. During a single foot raise test, the foot doctor will ask you to rise up on the tip of your toes while keeping your unaffected foot off the ground. If your posterior tendon has been attenuated or ruptured, you will be unable to lift your heel off the floor. In less severe cases, it is possible to rise onto your toes, but your heel will not invert normally. X-rays are not always helpful as a diagnostic tool for Adult Flatfoot because both feet will generally demonstrate a deformity. MRI (magnetic resonance imaging) may show tendon injury and inflammation, but can?t always be relied on for a complete diagnosis. In most cases, a MRI is not necessary to diagnose a posterior tibial tendon injury. An ultrasound may also be used to confirm the deformity, but is usually not required for an initial diagnosis.
Non surgical Treatment
Initial treatment is based on the degree of deformity and flexibility at initial presentation. Conservative treatment includes orthotics or ankle foot orthoses (AFO) to support the posterior tibial tendon (PT) and the longitudinal arch, anti-inflammatories to help reduce pain and inflammation, activity modification which may include immobilization of the foot and physical therapy to help strengthen and rehabilitate the tendon. 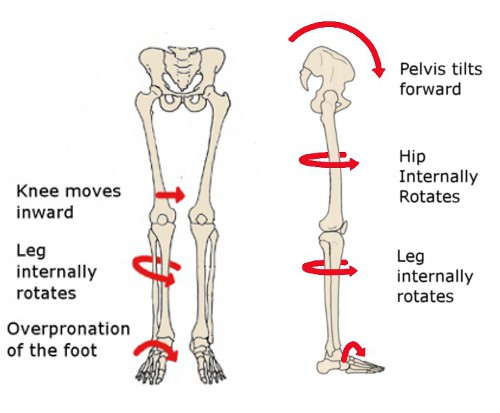
Surgical Treatment
Many operations are available for the treatment of dysfunction of the posterior tibial tendon after a thorough program of non-operative treatment has failed. The type of operation that is selected is determined by the age, weight, and level of activity of the patient as well as the extent of the deformity. The clinical stages outlined previously are a useful guide to operative care (Table I). In general, the clinician should perform the least invasive procedure that will decrease pain and improve function. One should consider the effects of each procedure, particularly those of arthrodesis, on the function of the rest of the foot and ankle.